Survey reveals the need for stronger mental health recovery infrastructure
The ICF COVID-19 Monitor Survey of U.S. Adults measures American attitudes and behaviors about COVID-19 and will track how they change over time. Here’s our first look at the mental health impacts of the pandemic. Learn more about the ICF COVID-19 Monitor Survey of U.S. Adults.
At the end of March, with near-record levels of unemployment reported and an increasing number of deaths due to COVID-19, many Americans reported experiencing symptoms of anxiety and depression. This article takes a deeper look at the mental health of Americans in the early days of the pandemic’s spread across the U.S., including relationships to economic and health outcomes and substance use.
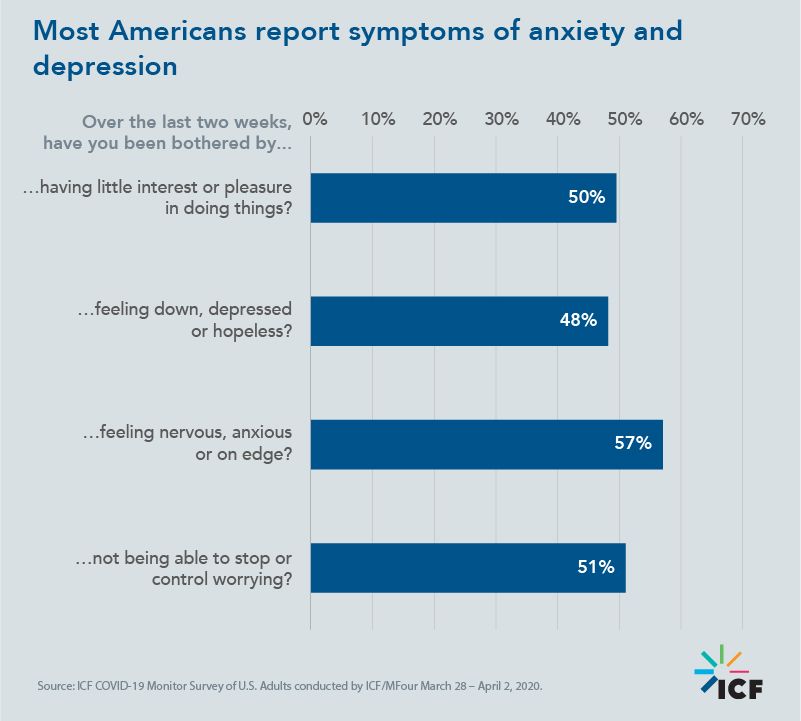
At the end of March, most Americans had experienced some symptoms of depression or anxiety in the past two weeks.
Stay at home orders were put in place in mid-March and quickly swept the nation. When this data was collected, Americans were still adjusting to this new and challenging reality. Not surprisingly, many reported symptoms of anxiety and depression. In fact, 70% of Americans reported experiencing anxiety- or depression-related symptoms in the past two weeks. The specific percentage of Americans reporting symptoms is shown below:
Exposure to and concern about the spread of the coronavirus is tied to more reported days of bad mental health.
Trying to get tested for COVID-19, being diagnosed with COVID-19, having greater concern for family, and higher perceived likelihood of getting sick were all significantly related to more reported days of bad mental health.
- Americans trying to get tested for COVID-19 reported an average of 3.11 bad mental health days in the past 7 days. Those who weren’t trying to get tested reported 1.56 bad mental health days in the same timeframe.
- Americans receiving a confirmed diagnosis of COVID-19 reported 4.75 average bad mental health days in the past 7 days, compared to 1.93 if another member of the household was diagnosed and 1.62 if no one in the household was diagnosed.
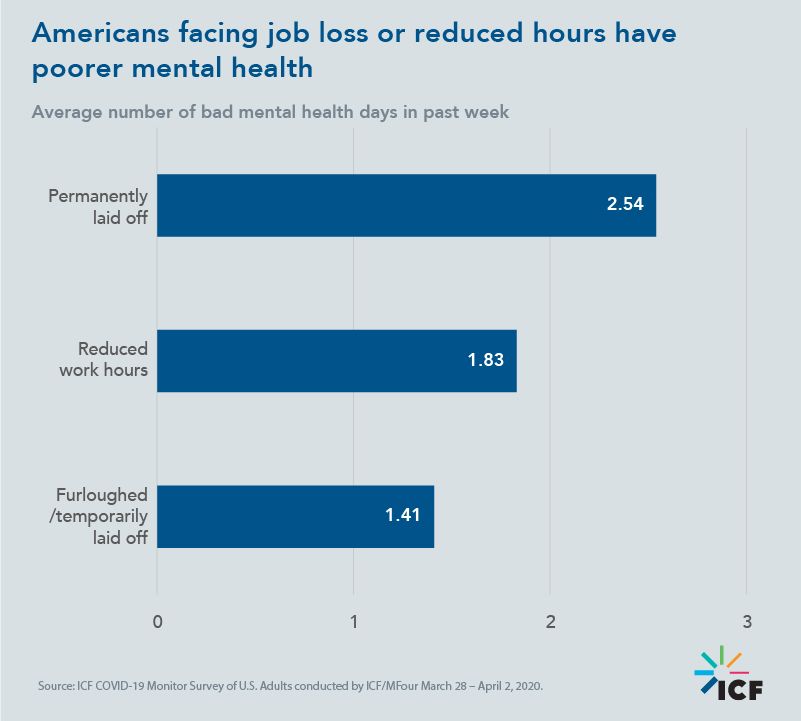
Job loss and increased financial burdens due to coronavirus worsen mental health.
As of late March, nearly 6 million Americans reported losing a job either permanently or temporarily. The permanent loss of a job or reduction in work hours was related to poorer mental health.
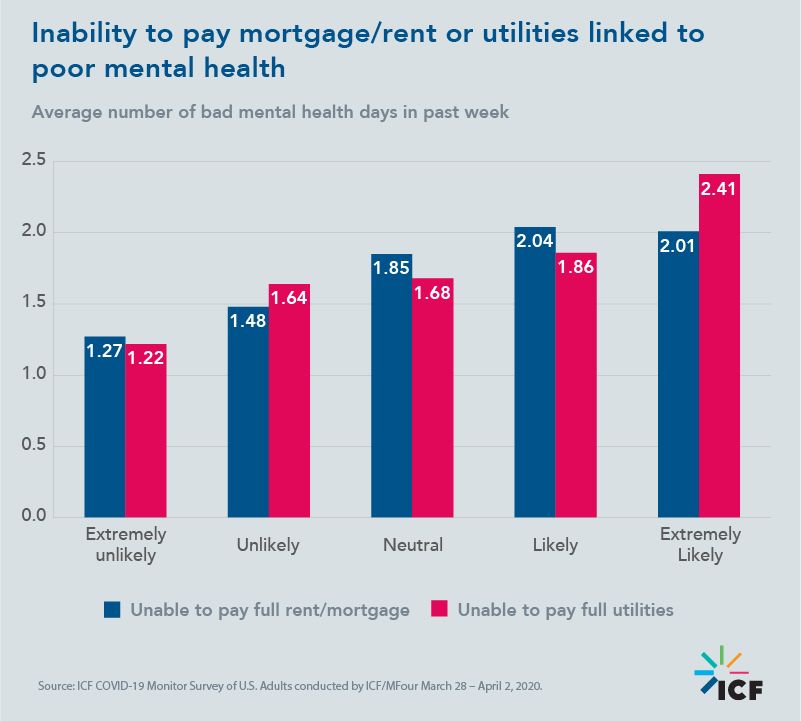
In addition, the expected inability to pay mortgage/rent and utilities in full in the next three months was related to poorer mental health.
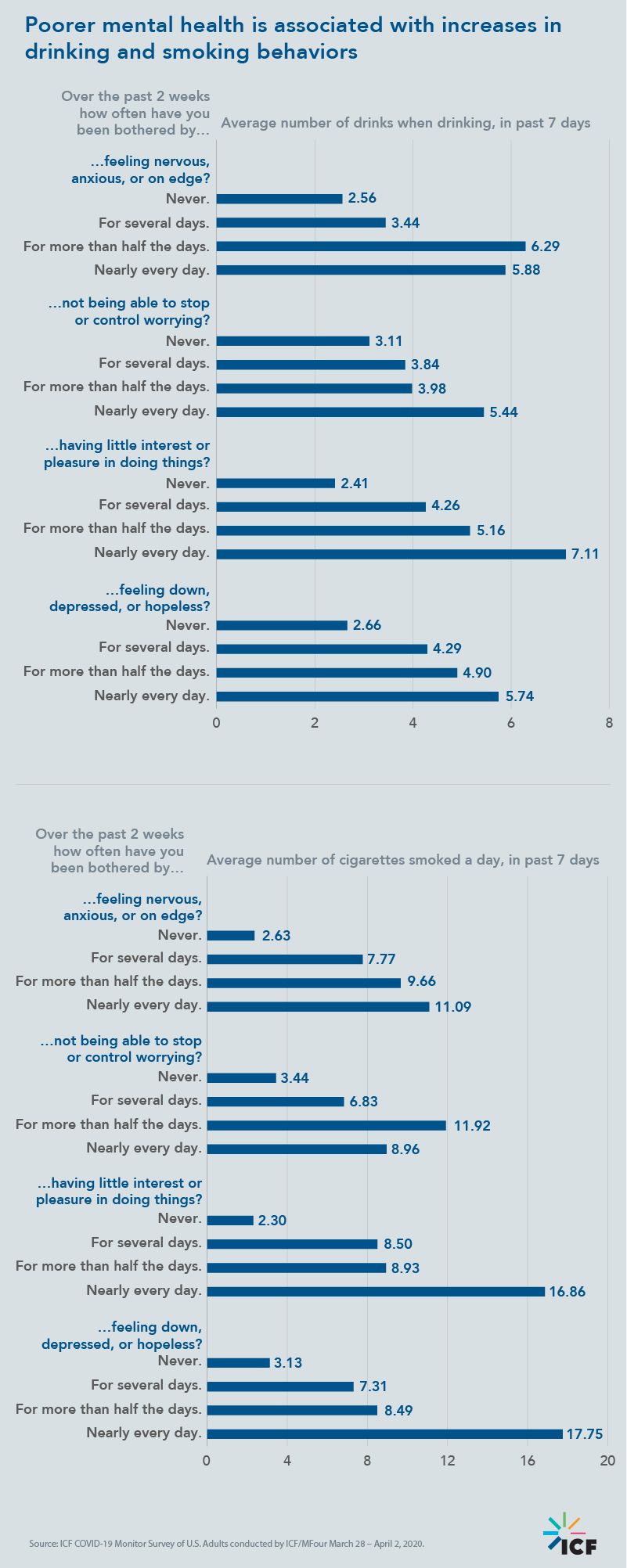
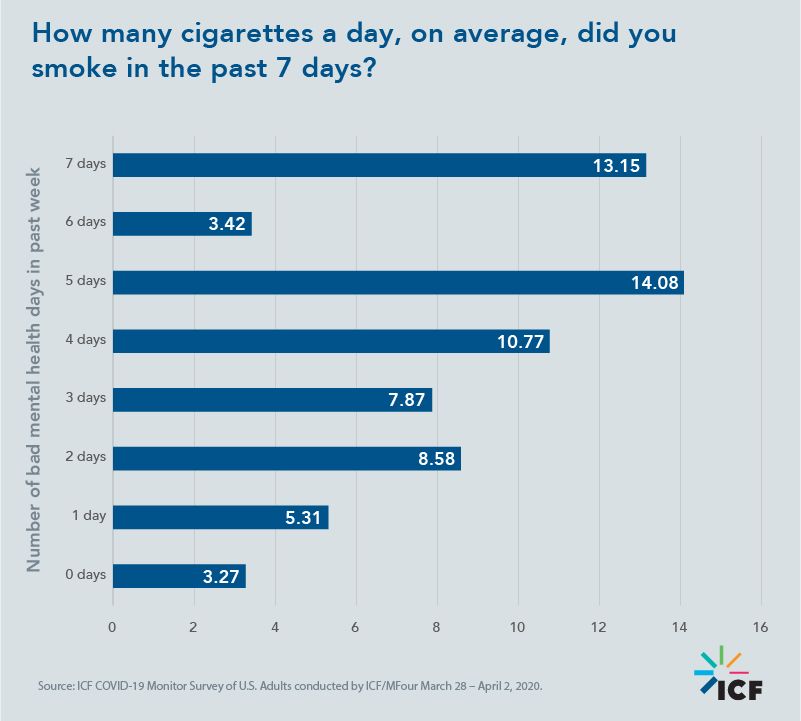
Poorer mental health leads to increased smoking and drinking.
Due to financial and health strains caused by the coronavirus, more Americans are reporting poorer mental health. Poorer mental health is associated with increases in smoking and drinking behaviors.
Overall, those who experienced greater frequency of depressive or anxious symptoms on a regular basis over the past two weeks smoked more and consumed more drinks on the days they drank.
Policy implications
As public health officials respond to the COVID-19 crisis and its aftermath, it is paramount that they recognize and attend to the mental health and substance use needs of citizens in the short-, medium-, and longer-term. While physical health and safety is a proximal priority, public health officials need to assess and fortify the current infrastructure to attend to Americans’ pronounced residual behavioral health needs.
Data that identifies the magnitude and circumstance of those needs provides a metric against which to benchmark behavioral health support and response capacity. For example, in the context of these findings, is the mental health and substance abuse workforce available and prepared to respond? Are crisis support services mobilized and ready across the country? And has the rapid pace of tele(primary)medicine deployment during this period of social distancing been as easy to adopt and deploy in the behavioral health fields?
Data-informed policies must expand, modify, and/or redeploy the behavioral health support and service infrastructure in our country to better respond to the public’s mental health and substance use needs in the face of COVID-19.
Watch this space
How will mental health and substance use behaviors change as the crisis evolves? Are the darkest days behind us, or is the worst yet to come? And how should public health officials be thinking about these findings and using them to inform effective policies? We will continue to share results from our data collection efforts over the coming weeks and encourage public health officials to bear this information in mind as you shape your response to COVID-19. Sign up to receive alerts as we roll out upcoming results and package our insights into reports.
Read other insights in the ICF COVID-19 Monitor Survey of U.S. Adults series.
